Nyere analyser og studier har skapt håp om å beskytte menneskeheten mot antibiotikaresistens som raskt blir en global trussel.
Oppdagelsen av antibiotika in mid 1900s was a significant milestone in the history of medicine as it was a miracle therapeutic for many bakteriell infeksjoner og bakterie-causing diseases. antibiotika were once termed as a “wonder drug” and now antibiotics are indispensable in both basic healthcare and advanced medical care and technology as they have really changed the world by protecting lives and being an essential part of treating various medical conditions and asassisting in critical surgical procedures.
Antibiotikamotstanden vokser i et raskt tempo
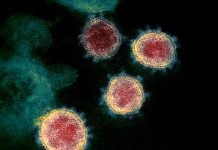
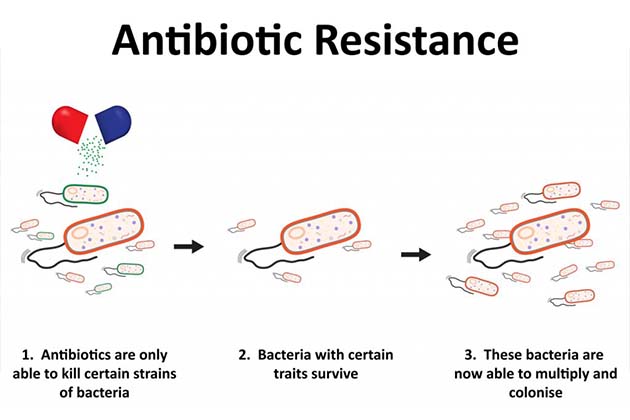
antibiotika are medicines which are naturally produced by microorganisms and they stop or kill bakterie from growing. It is of critical importance because bakteriell infections have plagued mankind throughout time. However, “resistant” bakterie develop defences that protect them against the effects of antibiotika when previously they were killed by them. These resistant bacteria then are able to withstand any attacks by antibiotics and consequently if these bakterie are disease-causing standard treatments stop working for that disease persisting the infections which can then easily spread to others. Thus, the “magical” antibiotics have unfortunately started to fail or started becoming ineffective and this is posing immense threat to the healthcare system worldwide. The number of resistant bakterie already cause more than 500,000 deaths every year and are eroding the efficiency of antibiotics for prevention and cure by being a silent killer by residing in almost 60% of the world’s populations in some form. Antibiotikaresistens threatens our ability to cure many diseases like tuberculosis, pneumonia and carry out advances in surgeries, treatment of cancer etc. It is estimated that approximately 50 million people will die from antibiotic resistant infections by 2050 and the day might actually come when antibiotika can no longer be used for treating critical infections the way they are being used now. This issue of antibiotic resistance is now an important health topic which needs to be addressed with a sense of urgency for a better future and the medical and scientific community and the governments worldwide are taking several steps toward achieving this goal.
WHOs undersøkelse: "post-antibiotika-æraen"?
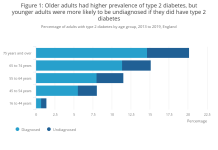
Verdens helseorganisasjon (WHO) har erklært antibiotikaresistens et høyt prioritert og alvorlig helseproblem gjennom sitt Global Antimicrobial Resistance Surveillance System (GLASS) som ble lansert i oktober 2015. Dette systemet samler inn, analyserer og deler data om antibiotikaresistens over hele verden. Fra og med 2017 har 52 land (25 høyinntekts-, 20 mellominntektsland og syv lavinntektsland) registrert seg i GLASS. Det er en første rapport1 inneholder informasjon om antibiotikaresistensnivåer levert av 22 land (en halv million deltakere registrert i undersøkelsen) som viser vekst i en alarmerende hastighet – totalt sett en enorm resistens på 62 til 82 prosent. Dette initiativet fra WHO har som mål å skape bevissthet og koordinere mellom ulike nasjoner for å takle dette alvorlige problemet på globalt nivå.
Vi kunne ha forhindret antibiotikaresistens og kan fortsatt
How did we reach this phase of humanity where antibiotic resistance has turned into a global threat? The answer to that is quite simple: we have extremely overused and misused antibiotika. The doctors have overly prescribed antibiotika to any or every patient in the past many decades. Also, in many countries, especially the developing countries of Asia and Africa, antibiotika are available over-the-counter at the local pharmacist and can be purchased without even requiring a doctor’s prescription. It is estimated that 50 percent of the time antibiotika are prescribed for virus-causing infection where they basically do no good because the virus will still complete its life span (generally between 3-10 days) whether antibiotika are taken or not. In fact, it’s just incorrect and a mystery for many as to how exactly antibiotika (which target bakterie) will have any effect on viruses! The antibiotika could ‘maybe’ relieve some symptoms associated with the viral infection. Even then this continues to be medically unethical. The correct advice should be that since no treatment is available for most viruses, the infection should just run its course and in the future these infections should be alternatively prevented by following strict hygiene and keeping one’s environment clean. Furthermore, antibiotika are being routinely used in enhancing agricultural output worldwide and feeding to livestock and food-producing animals (chicken, cow, pig) as growth supplements. By doing so humans are also put to huge risk of ingesting antibiotic-resistant bakterie which reside in those food or animals causing rigorous transfer of resistant strain bakterie over grenser.
Dette scenariet kompliseres ytterligere av det faktum at ingen nye antibiotika har blitt utviklet av farmasøytiske selskaper de siste tiårene – den siste nye antibiotikaklassen for gramnegative bakterie ble kinolone utviklet for fire tiår siden. Slik vi er nå, kan vi egentlig ikke tenke på å forebygge antibiotikaresistens ved å tilsette flere og forskjellige antibiotika da dette bare vil komplisere resistens og overføring ytterligere. Mange medikament selskaper har påpekt at utvikling av nye medikament er for det første veldig dyrt da det er en lang prosess som krever enorme investeringer og potensiell fortjeneste fra antibiotika is generally very low that the companies are unable to ‘break even’. This is convoluted by the fact that a resistant strain would develop for a new antibiotic somewhere in the world within two years of its launch since no legal framework is in place to curb antibiotic overuse. This doesn’t exactly sound hopeful from a commercial as well as a medical point of view and thus developing new antibiotika is not the solution for prevention of their resistance.
WHO anbefaler handlingsplan2 for å forhindre antibiotikaresistens:
a) Healthcare professionals and workers should be doing a careful detailed assessment before prescribing antibiotika to humans or animals. A Cochrane review of various methods3 aimed at reducing antibiotic abuse in any clinical set up has concluded that the ‘3-day prescription’ method was fairly successful, in which the patient suffering from an infection (which is not bakteriell) is conveyed that his/her condition will improve in 3 days, else antibiotika can be taken if symptoms get worse – which generally don’t since the viral infection has run its course by that time. b) The general public should be confident to ask questions when they are being prescribed antibiotika and they must take antibiotika only when satisfied that it is absolutely necessary. They must also complete the prescribed dosage to prevent fast growth of resistant bakteriell strains. c) Agriculturists and livestock breeders should follow a regulated, limited use of antibiotics and do so only where it matters (eg. to treat an infection). d) Governments should setup and follow national level plans to curb antibiotic use1. Det må settes opp skreddersydde rammer for utviklede land og mellom- og lavinntektsland i forhold til deres behov.
Nå som skaden er gjort: takle antibiotikaresistens
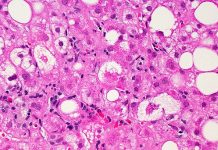
So that we do not plunge into a new ’post antibiotika’ era and return to the pre-penicillin (first antibiotic to be discovered) era, lot of research is happening in this field loaded with failure and occasional successes. Recent multiple studies show ways to tackle and maybe reverse antibiotic resistance. The first study published in Journal of Antimicrobial Chemotherapy4 viser at når bakterie become resistant, one of the ways which they adopt to restrict antibiotika action is by producing an enzyme (a β-lactamase) which destroys any antibiotic that is trying to get into the cell (for treatment). Thus, ways to inhibit the action of such enzymes could successfully reverse antibiotic resistance. In a second subsequent study from the same team at University of Bristol, UK but in collaboration with University of Oxford published in Molekylær mikrobiologi5, they analysed the effectiveness of two types of inhibitors of such enzymes. These inhibitors (from the bicyclic boronate class) were seen to be very effective on a particular type of antibiotic (aztreonam) such that in the presence of this inhibitor, the antibiotic was able to kill many resistant bakterie. Two of such inhibitors avibactam and vaborbactam – are now undergoing clinical trial and have been able to save a life of a person suffering from untreatable infection.The authors have succeeded with only a particular type of antibiotika, ikke desto mindre har arbeidet deres skapt håp om å snu strømmen av antibiotikaresistens tilbake.
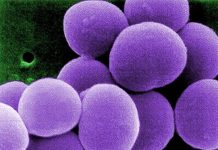
I en annen studie publisert i Vitenskapelige rapporter6, har forskere ved Université de Montréal utviklet en ny tilnærming for å blokkere overføring av resistens mellom bakterier, som er en av måtene antibiotikaresistensen sprer seg på sykehus og helseavdelinger. Genene som er ansvarlige for å gjøre bakteriene resistente er kodet på plasmider (en liten DNA fragment som kan replikere uavhengig) og disse plasmidene overføres mellom bakteriene, og sprer dermed de resistente bakterie nært og fjernt. Forskere undersøkte beregningsmessig et bibliotek av små kjemiske molekyler som ville binde seg til proteinet (TraE) som er essensielt for denne plasmidoverføringen. Inhibitorbindingsstedet er kjent fra proteinets 3D molekylære struktur, og det ble sett at når potensielle hemmere ble bundet til proteinet, ble overføringen av antibiotikaresistente, genbærende plasmider betydelig redusert, og antydet dermed en potensiell strategi for å begrense og reversere antibiotika. motstand. Men for denne typen studier 3D molekylær struktur av et protein er nødvendig, noe som gjør det litt begrensende ettersom mange proteiner ennå ikke er strukturelt karakterisert. Likevel er ideen oppmuntrende, og slike hemmere kan sannsynligvis spille en viktig rolle i det daglige helsevesenet.
Antibiotikaresistens truer og undergraver flere tiår med forbedringer og gevinster som er gjort i menneskelig helsetjenester og utvikling and implementation of this work will have a huge direct impact on the capability of people to live healthy lives.
***
{Du kan lese den originale forskningsoppgaven ved å klikke på DOI-lenken nedenfor i listen over siterte kilder}
Source (s)
1. HVEM. Globalt overvåkingssystem for antimikrobiell resistens (GLASS) rapport. http://www.who.int/glass/resources/publications/early-implementation-report/en/ [Åpnet 29. januar 2018].
2. HVEM. Hvordan stoppe antibiotikaresistens? Her er en WHO-resept. http://www.who.int/mediacentre/commentaries/stop-antibiotic-resistance/en/. [Åpnet 10. februar 2018].
3. Arnold SR. og Straus SE. 2005. Intervensjoner for å forbedre antibiotikaforskrivningspraksis i ambulant omsorg.Cochrane Database Syst Rev. 19 (4). https://doi.org/10.1002/14651858.CD003539.pub2
4. Jiménez-Castellanos JC. et al. 2017. Envelope-proteomendringer drevet av RamA-overproduksjon i Klebsiella pneumoniae som forbedrer ervervet β-laktamresistens. Journal of Antimicrobial Chemotherapy. 73(1) https://doi.org/10.1093/jac/dkx345
5. Calvopiña K. et al.2017. Strukturell/mekanistisk innsikt i effektiviteten av ikke-klassiske β-laktamase-hemmere mot kliniske isolater med omfattende medikamentresistente Stenotrophomonasmaltophilia. Molekylær mikrobiologi. 106(3). https://doi.org/10.1111/mmi.13831
6. Casu B. et al. 2017. Fragmentbasert screening identifiserer nye mål for hemmere av konjugativ overføring av antimikrobiell resistens av plasmid pKM101. Vitenskapelige rapporter. 7 (1). https://doi.org/10.1038/s41598-017-14953-1